Virtual reality as an adjunctive comfort measure in the intensive care and coronary care unit: A nurse-led quality improvement project
Katherine A. Kissel, MN, RN, CNCC(C), ACCN, Andrea Soo, PhD, and Kimberley Tateson Bennett, RN
Abstract
Background: Pain, discomfort, and anxiety in critical care units are complex, multifaceted experiences. Nurse-led implementations of adjunctive comfort measures in critical care settings are essential components in the holistic management of these experiences. Virtual reality is gaining popularity as an adjunctive comfort measure across acute care settings to promote patient comfort, though there is limited evidence examining the utility of virtual reality in critical care.
Purpose: Firstly, to determine if virtual reality, as a nurse-led adjunctive comfort measure, improved patient self-reported pain, discomfort and relaxation. Secondly, to identify if virtual reality led to significant alterations in patient physiological variables.
Methods: A quality improvement project was performed with intensive care and coronary care unit patients receiving virtual reality immersion. Pre and post-tests measured self-reported pain, relaxation, and general/overall discomfort. We examined pre and post vital signs and adverse outcomes (nausea, dizziness, eye strain/discomfort). We used paired t-tests to compare outcomes pre and post virtual reality.
Results: Post virtual reality, patient (n = 13) scores showed significant reductions in pain (mean improvement: 1.04, 95% CI [0.45, 1.62]), relaxation (mean improvement: 3.08, 95% CI [0.45, 0.62]), general/overall comfort (mean improvement: 2.08, 95% CI [0.86, 3.30]), and respiratory rate (mean reduction: 1.54, 95% CI [0.22, 2.86]). There were no significant changes in adverse events or other physiological variables.
Conclusion: Virtual reality was deemed as a safe, effective adjunctive comfort measure within one intensive care unit and coronary care unit. Virtual reality may be a useful tool to reduce pain, discomfort, and improve patient relaxation in critical care settings, though research within this specialized population is needed.
Kissel, K.A., Soo, A., & Tateson Bennett, K. (2021). Virtual reality as an adjunctive comfort measure in the intensive care and coronary care unit: A nurse-led quality improvement project. The Canadian Journal of Critical Care Nursing, 32(4), 5-13. DOI: 10.5737/23688653-324513
Implications for Nursing
- Virtual reality as an adjunctive comfort measure, as well as a pain distractor, is gaining popularity, though evidence pertaining to its use within critical care is limited.
- This quality improvement project highlights the potential benefits of virtual reality as a nurse-led adjunctive comfort measure, and when used within defined parameters, significant improvements in patient pain, comfort and relaxation were observed.
- Research is needed to examine the use of virtual reality amongst larger, randomized, critical care populations, utilizing validated tools where applicable.
Background
Pain in the intensive care unit (ICU) is a complex phenomenon: underlying critical illness, chronic and comorbid conditions, the presence of invasive lines, and procedural pain (both related to medical and nursing procedures) all contribute to pain sources within the critical care environment (Devlin et al., 2018; Puntillo et al., 2014; Tracy & Chlan, 2011). Inadequate pain management in the ICU has been demonstrated to have adverse impacts on patients’ physiological and mental status. These alterations may negatively impact patient recovery and prolong ICU length of stay (Shahriari et al., 2015). Further, anxiety and pain are often interrelated. Some studies have found where patients experience increased pain scores, they also experience more severe symptoms of anxiety (Castillo et al., 2016; Filipovic-Grcic et al., 2010). Fear, underlying physiological conditions, sleep disturbance, and inability to communicate, as well as loss of control and the presence of mechanical ventilation, may further contribute to patient anxiety (Meghani et al., 2017; Rotondi et al., 2002; Tracy & Chlan, 2011). Pharmacological pain management in the ICU is often indicated, however, the excessive use of opiate analgesia and sedation are associated with increased risk of adverse patient outcome including respiratory depression, prolonged mechanical ventilation and increased length of stay in the ICU (Balzer et al., 2015; Devlin et al., 2018). In order to reduce such adverse outcomes, Devlin et al. (2018) highlight the need for ongoing, protocolized pain assessment and management, and recommend the use of adjunctive pharmacological and non-pharmacological therapies within the ICU.
In accordance with the Canadian Association of Critical Care Nurses (2017), critical care nurses play a key role in facilitating “optimal comfort and well-being in a highly technical environment” (p. 4). One way in which critical care nurses may independently promote patient comfort, reduce pain, or enhance the effectiveness of pharmacological approaches is through the implementation of adjunctive, or non-pharmacological, therapies (Meghani et al., 2017; Tracy & Chlan, 2011). An interest in the utility of specific adjunctive therapies to enhance patient outcomes is growing within the literature. In particular, the use of virtual reality (VR) is expanding across the acute care setting, with potential benefits cited as originating from the immersive nature of the VR environment (Dascal et al., 2017; Tashjian et al., 2017).
VR is defined as “an artificial environment… experienced through sensory stimuli… and in which one’s actions partially determine what happens in the environment” (Merriam-Webster, 2018). Within the inpatient healthcare setting, head mounted VR devices are becoming increasingly popular as they are easy to use and allow the user to customize their own experience through interaction with the virtual environment (Dascal et al., 2017; Mallari et al., 2019). Though numerous studies examine the impact of VR on patient outcomes, the level of evidence varies. Within two recent systematic reviews, it was noted that VR was a useful tool in the inpatient setting to provide pain distraction and reduce pain levels during painful procedures (Dascal et al., 2017; Mallari et al., 2019). VR may have further benefit in the reduction of chronic pain during or immediately post VR usage, however, evidence is limited regarding lasting analgesic effect (Jin et al., 2016). Additionally, few studies noted significant reduction in opiate use in patients undergoing painful procedures who utilize VR distraction compared to those who did not (McSherry et al., 2018; Pandya et al., 2017). Though Tashjian et al. (2017) also found VR to be an effective adjunctive therapy to reduce patient pain, they highlight that additional research is required to determine if VR as a meditative intervention may further promote patient comfort in acute care settings where patients often experience lack of control and routine.
Despite the growing body of literature, evidence regarding VR use as an adjunctive comfort measure within critical care remains limited (Devlin et al., 2018). To date, three publications were located which examined VR use in a critical care environment, though they lack transferability specific to the patient population within this project. At the time of project inception, one study reported that patients post cardiac surgery (n = 67) experienced reductions in pain levels (88%), and improvements in physiological variables post VR intervention (Mosso-Vázquez et al., 2014). These authors highlight VR was an effective method to safely reduce pain as an “additional support mechanism” through its distractive properties (p. 377). Two additional publications were located post project completion, including one case report in which VR was utilized to reduce patient anxiety while undergoing extracorporeal membrane oxygenation (Blair et al, 2019). The final noted in a feasibility study that VR was generally well tolerated by patients, provided environmental distraction, and promoted patient relaxation (Gerber et al., 2019). Recognizing the limited body of evidence examining VR application within critical care, it is important to further examine the use of VR within this setting.
Purpose
The overarching purpose of this quality improvement (QI) project was to determine if the use of virtual reality as an adjunctive comfort measure improved patient comfort in one ICU and one coronary care unit (CCU). Specific aims included whether the use of VR would lead to improvements in: patient self-reported pain, levels of overall discomfort, and relaxation. Secondary outcomes included whether the use of VR in the ICU and CCU would lead to reductions in physiological variables including heart rate, respiratory rate, and mean arterial pressure. Results of the project would be used to determine if a VR program could be immediately implemented within the ICU/CCU as an adjunctive patient comfort measure.
Methods
Quality Improvement Framework and Project Approval
The project was formulated utilizing a Plan, Do, Study, Act (PDSA) improvement framework (Institute for Health Care Improvement, 2021). Though the project met criteria for QI (including goal of immediate practice improvement in the defined setting), to further identify if a formal ethics committee review was required, the Project Ethics Community Consensus Initiative (ARECCI) Ethics Guideline and Screening Tools were completed (Alberta Innovates, 2017). The purpose of these tools is to aid teams in identifying the ethical risks and management strategies associated with non-research projects (Alberta Innovates, 2017). Based on scoring recommendation, a formal ARECCI second opinion review was obtained. This second opinion review further determined project submission to a formal ethics review board was not required.
Senior Administrative Leadership within Alberta Health Services and the Medical Directors for both Intensive Care and Coronary Care within the departmental portfolios provided approval for this project. Consideration of patients’ safety, dignity, anonymity, and protection from coercion was incorporated into the project design. Informed consent was obtained prior to commencing individual trial. Consent script was utilized to ensure consistency and to ensure all information was covered prior to eliciting consent from patients.
Design
We utilized a pre-post survey for the project to determine if use of a VR application reduced pain and discomfort, and improved relaxation in the critical care patient population. Through the PDSA framework, each patient survey was reviewed. Based upon survey results and patient reported experience, it was deemed no further PDSA cycles were required.
Sample
Convenience sampling from the patients admitted to the ICU or CCU occurred between May 2018 and January 2020. In order to be able to validate results from the data collected, we had originally aimed to include approximately 30 patients for this project. However, due to time restraints, and unanticipated barriers to VR application (device access, facilitator model, workload, environmental demands and priority needs of the ICU/CCU), we were only able to survey a smaller sample of patients.
Recruitment
Initially, unit nurses were provided education regarding the VR project in order to support patient recruitment and enrollment, with a trained volunteer to support device setup one day per week. However, when patients were identified, volunteers were unavailable, and no patients were enrolled. Subsequently, to ensure suitable enrollment into the project, patients were approached and verbally invited to participate by a Clinical Nurse Educator (CNE) or Clinical Resource Nurse (CRN) based on their knowledge of inclusion and exclusion criteria and device training. Patients were given a brief description of the VR intervention and if they were interested in participating, verbal consent was obtained (as deemed appropriate through the ARECCI second opinion review). A single page of information was shared with prospective patients to provide an image of the VR environment as well as potential triggers within the environment (e.g., fire burning in fire pit, animals found in the forest). Patients were informed of the purpose of the trial as well as potential adverse effects in order to make an informed decision.
Inclusion/exclusion criteria
Inclusion criteria will encompass the patient being; awake, alert, oriented, cooperative, hemodynamically stable, and must be able to sit in high-fowlers position and have trunk/abdominal control, ability to interact with the VR environment, operate the VR remote (or at minimum remove the device from their face), and identify relevant fears/triggers to avoid within the VR environment.
In addition to absence of inclusion criteria, the following excluded patients from VR usage for project purposes: hemodynamic instability including active chest pain, pre-existing or predisposition to nausea/vertigo, motion sickness for any intubated patient or patient deemed an aspiration risk, susceptibility to claustrophobia, presence of active dementia, alternative neurological/cognitive disturbances including delirium, recent stroke, seizure disorder, psychiatric disorders, facial injury rendering the patient unable to wear the VR device, absence of audiovisual aids (i.e., hearing aids/glasses), isolation precautions, or non-English speaking.
Consideration of inclusion and exclusion criteria were established to control for confounding variables. For example, timing of VR was intentionally delayed around administration of analgesia to avoid possible attribution of analgesia to change in self-reported scores. Further, the pre-test was performed immediately prior to intervention and the post-test completed immediately after intervention in an effort to capture changes in self-reported scores.
Setting
The project was performed in the participant’s room within the ICU or CCU. Patients were required to be either in bed, sitting in high-fowlers position, or in a stationary chair for the duration of the trial. VR immersion lasted between 10 – 20 minutes with the option to discontinue at any time.
Intervention
The intervention was the VR application environment consisting of an animated, interactive, virtual space that also included guided meditation and background music. The VR experience featured a quiet nature scene and was selected for three main reasons. Firstly, the overall theme of the app which was promoted as calm and relaxing. Secondly, simplicity of the experience did not pose some of the issues that other more realistic or game-based VR experiences may provide (e.g., rapid profile movements, fear of heights/water submersion, interaction with natural elements, etc.). Thirdly, minimal patient engagement with the environment was required due to the presence of invasive lines (e.g., avoiding significant head movements).
Procedure
After verbal consent was obtained, the pre-test questionnaire was completed by the patient, with vital signs being completed by the CNE or CRN. Orientation to the remote control was provided prior to the patient donning the VR headset. Once the VR headset was placed, the patient was guided through setup on the VR app. Unless the patient had requested to stop the immersion, the nurse would ask them at the 10-minute mark if they wanted to continue for up to an additional 10 minutes (20 minutes total immersion time). After completion of the VR immersion, the post-test questionnaire was completed and the CNE or CRN obtained a second set of vital signs. In order to ensure patient safety and monitor for adverse effects of immersion (nausea, eye strain, dizziness) the CNE or CRN continuously monitored the patient for the duration of the trial.
Outcomes
The primary outcomes were self-reported scores regarding: pain, relaxation, and discomfort. Pre-test, post-test questionnaires were created for ease and usability. Pain assessment and relaxation were placed on the zero-to-10-point scale (McSherry et al., 2018). The term relaxation was used instead of anxiety, to avoid clinically implicit language as well as effects of polarizing terminology with patients (Tate et al., 2012). There are many validated tools to measure anxiety, relaxation, and mindfulness. However, given the scope of this QI project, none were deemed appropriate due to complexity. The self-reported measure of discomfort was placed on a Likert scale of 7 based on agreement with a statement (1 = strongly disagree, 2 = disagree, 3 = somewhat disagree, 4 = neither agree nor disagree, 5 = somewhat agree, 6 = agree, 7 = strongly agree). A 7-point Likert scale was selected for simplicity, ease of use, and increased accuracy of reporting (Finstad, 2010).
Secondary outcomes were monitoring for adverse events including nausea, dizziness, and eye strain/discomfort, as well as changes to vital signs before and after a VR intervention. A 7-point Likert scale based on degree of agreement with a statement (as outlined above) was used to measure adverse event outcomes. In addition to the self-rating component of the survey, patients were given the option to capture thoughts, feelings, or comments in an optional free text response. Utilization of current literature was used to guide and develop appropriate criteria and consideration to ensure safety of patients (Bruck & Watters, 2011; Nichols & Patel, 2002; Tashjian et al., 2017).
On the post-test questionnaire, four additional questions were asked (7-point Likert scale); three questions specifically targeted the VR environment (realness of environment, interest in further VR experiences, and recommendation to others) and one addressed sense of overall comfort.
Data Analysis
Descriptive statistics were utilized to report results using frequencies with percentages, means with standard deviations (SD) or medians with interquartile ranges (IQR), as appropriate. Data was analyzed using R, version 4.0.0 (R Core Team, 2020). Paired t-tests were used to compare primary and secondary outcomes pre- and post-VR. Boxplots were utilized to review the distributions of differences in pre- and post-VR scores. As not all distributions were relatively symmetrical, sensitivity analyses were also done using Wilcoxon signed ranked tests.
Results
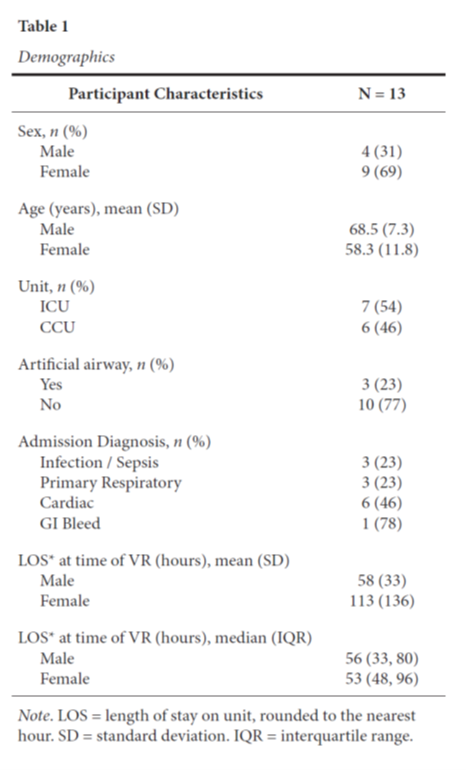
Thirteen patients met the eligibility criteria and consented to participate in the VR trial between May 2018 and January 2020. As this was a QI initiative, the number of individuals excluded or whom declined to participate were not tracked. Reasons for exclusion included: presence of isolation precautions, and on one occasion, patient reported fear of environmental triggers. Of the 13 patients, 4 (31%) were male with a mean age of 68.5 years (SD = 7.33), and 7 (69%) were female with a mean age of 58.3 years (SD = 11.77). Primary admission diagnoses were: 46% cardiac (n = 6), 23% respiratory (n = 3), 23% sepsis (n = 3), and 8% gastro-intestinal bleed (n = 1) (Table 1).
VR Immersion
Mean duration in VR was 15.5 minutes (SD = 4.7). Six (46%) patients competed the full 20-minute immersion. Of the 7 sessions discontinued prior to maximal allotted time, where recorded (n = 3), reasons cited for early discontinuation were: interruption for patient rounds (n = 1), toileting requirements (n = 1), and post session report of inability to hear audio (n = 1). No patient requested early discontinuation due to undesired effects including presence of, or increase in nausea, dizziness, or eye strain/discomfort. Post survey results reported no occurrence of other adverse event or patient deterioration.
Primary Results
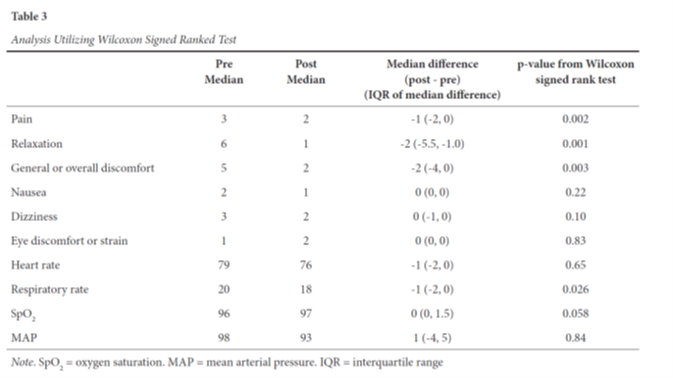
Analyses comparing outcomes pre-post VR are in Tables 2 and 3, respectively. All three primary outcomes (pain, relaxation and general/overall comfort scores) demonstrated statistically significant improvement post VR. Pain scores improved in 8 (61.5%) patients with a mean improvement of 1.04 (95% confidence interval [CI], (0.45, 1.62], p = 0.002). Relaxation scores improved in 12 (92.3%) patients with a mean improvement of 3.08 (95% CI [1.66, 4.50], p = 0.001). General/overall comfort scores improved in 9 (69.2%) patients with a mean improvement of 2.08 (95% CI [0.86, 3.30], p = 0.003). No significant changes were noted to the secondary (adverse) outcomes including nausea (p = 0.22), eye discomfort or strain (p = 0.83), and dizziness (p = 0.10). Any report of condition improvement or worsening within these secondary outcomes was a result of minor progression along the Likert scale, with no large swings from the disagreement to agreement categories, or vice versa. Of the physiological variables, respiratory rate was the only variable in which a significant change was noted (7.5% reduction, or mean decrease of 1.54, 95% CI [0.22, 2.86], p = 0.026). No significant change was noted to heart rate (p = 0.65) or mean arterial pressure (p = 0.84) post VR. There was an observed trend towards increasing SpO2 post VR, though this was not statistically significant (p = 0.058). The analysis of SpO2 was based upon a sample of 11, as SpO2 recordings were incomplete for two patients.
Post-Only Survey Results
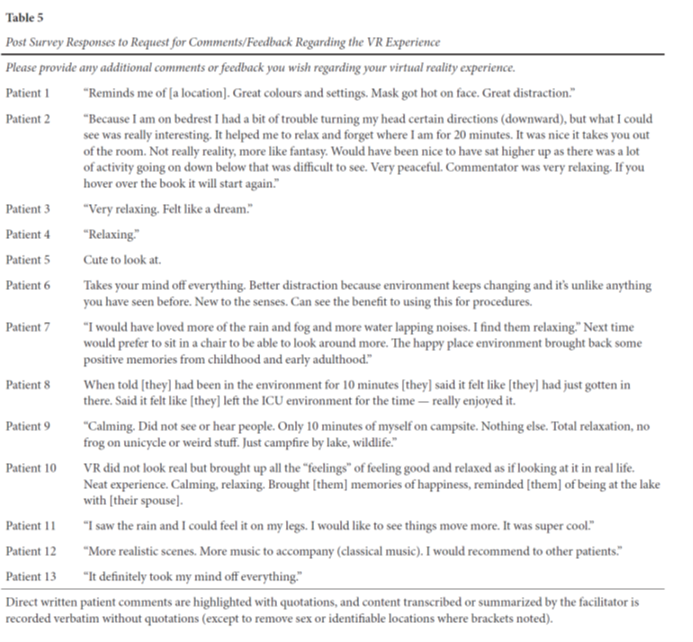
Of post-survey data results, questions pertaining to immersion, and the general VR experience are summarized in Table 4. In alignment with self-reported findings of improved general/overall discomfort post VR, 92.3% of patient agreed that their VR experience improved [their] sense of overall comfort (somewhat agree, agree, strongly agree). Finally, participants were offered to provide addition comments or feedback regarding their virtual reality experience. Responses, where provided, are summarized in Table 5. Key themes included annotated experiences of relaxation, distraction/escape, and nostalgia in relation to past experiences.

Discussion
The overarching purpose of this project was to determine if the use of virtual reality as an adjunctive comfort measure improved patient comfort in the ICU and CCU setting. Our findings demonstrated that utilizing VR as a nurse-led adjunctive comfort measure did reduce self-reported levels of pain and discomfort, while improving relaxation. No adverse events, including significant increases in nausea, dizziness, or eye strain/discomfort were reported. No significant change was noted to the vital signs (with the exception of respiratory rate) post VR. Self-reported findings were further reinforced by anecdotal post session comments. These comments further align with previous VR literature including improved sense of well-being, increased relaxation, environmental distraction, and a decrease in pain.
VR applications are expanding across the acute care setting. While current gaps exist within the critical care literature pertaining to the use of VR as a comfort measure, this quality improvement project highlights the potential utility of VR in these specific critical care environments. Given the linkages between physiological and environmental alterations that occur within the critical care unit and patient experiences of pain and anxiety, implementation of non-pharmacological interventions are essential to support patient well-being (Meghani et al., 2017; Tracy & Chlan, 2011). Critical care nurses play an integral role in supporting this provision of non-pharmacological interventions (Canadian Association of Critical Care Nurses, 2017; Tracy & Chlan, 2011). Through this project, VR may be considered as a potential non-pharmacological measure in promoting patient comfort. Although our sample was small, the data supports expanded implementation of a VR program in this ICU/CCU.

This QI project has numerous limitations. The small convenience sample obtained for purposes of this project within one ICU and CCU limits generalizability. The priority demands of the critical care unit and time required to facilitate VR (50-60 minutes per participant) led to missed VR opportunities. It was identified device location (i.e., increased accessibility on unit), training related to device setup, and a quick reference tool were essential to facilitate project enrollment.
Unlike the other physiological variables, the reduction of respiratory rate was noted to be statistically significant (mean reduction 1.54 breaths per minute), however, the clinical significance of this reduction is unknown. Research examining the relationship between VR, pain, comfort, relaxation, and respiratory rate in the critical care setting is warranted. Though the term relaxation was used for the purposes of this project, additional investigation regarding the impact of VR on patient anxiety utilizing a validated anxiety assessment tool would be beneficial. Of interest are also the subjective or annotated comments which speak to key themes of: relaxation, calmness, and environmental distraction or escape. Research would be beneficial to explore the relationships between pain and environmental distraction in a highly technical care environment. Finally, though significant improvements were noted to patient reported pain, discomfort, and relaxation scores post VR, long-term benefit of these outcomes remain unknown.
Conclusion
Within one ICU and CCU, virtual reality, as nurse-led adjunctive comfort therapy, was found to be a safe, successful, and desirable tool to reduce patient reported pain, general/overall discomfort, and improve relaxation. Research, with larger sample sizes, the use of validated assessment tools (where applicable), and examination of long-term benefit of VR is required within the critical care setting.
Author Notes
Katherine A. Kissel, MN, RN CNCC(C), ACCN(C), Clinical Nurse Specialist, Alberta Health Services, Calgary, Alberta.
Andrea Soo, PhD, Senior Biostatistician, Department of Critical Care Medicine, Alberta Health Services, and Adjunct Assistant Professor, Department of Critical Care Medicine, Cumming School of Medicine, University of Calgary, Calgary, Alberta.
Kimberley Tateson Bennett, RN, Director of Health, CUPS, Calgary, Alberta.
Address for correspondence
Katherine Kissel, Intensive Care Unit, Peter Lougheed Centre, 3500 26 Ave NE, Calgary, AB T1Y 6J4.
Email : katherine.kissel@albertahealthservices.ca Phone : 403-943-4544
Funding and conflict of interest statement
The authors have no funding and conflict of interest to disclose. The authors are the recipients of the Spacelabs Innovative Project Award (2021) through CACCN.
REFERENCES
Alberta Innovates (2017). ARECCI Ethics Guideline Tool. Retrieved from: https://albertainnovates.ca/wp-content/uploads/2017/11/ARECCI-Ethics- Guideline-Tool.pdf
Blair, G.J., Kapil, S., Cole, S.P., & Rodriguez, S. (2019). Virtual reality use in adult ICU to mitigate anxiety for a patient on V-V ECMO. Journal of Clinical Anesthesia, 55, 26-27.doi:10.1016/j.jclinane.2018.12.033
Balzer, B., F., Wieb, B., Kumpf, O., Trekatsch, S., Spies, C., Wernecke, K.-D., Krannich, A., & Kastrup, M. (2015). Early deep sedation is associated with decreased in-hospital and two-year follow-up survival. Critical Care, 19(197), 1-9. doi:10.1186/s13054-015-0929-2
Bruck, S., & Watters, P. A. (2011). The factor structure of cybersickness. Displays, 32(4), 153- 158. Doi:10.1016/j.displa.2011.07.002
Canadian Association of Critical Care Nurses. (2017). Standards for Critical Care Nursing Practice (5th ed.). Retrieved from: https://caccn.ca/wpcontent/uploads/2019/05/STCACCN-2017-Standards-5th- Ed.pdf
Castillo, M. I., Cooke, M., Macfarlane, B., & Aitken, L. M. (2016). Factors associated with anxiety in critically ill patients: A prospective observational cohort study. International Journal of Nursing Studies, 60, 225-233. doi:10.1016/j.ijnurstu.2016.05.007
Dascal, J., Reid, M., Ishak, W. W., Spiegel, B., Recacho, J., Rosen, B., & Danovitch, I. (2017). Virtual reality and medical inpatients: A systematic review of randomized, controlled trials. Innovations in Clinical Neuroscience, 14(1-2), 14-21.
Devlin, J. W., Skrobik, Y., Gélinas, C., Needham, D. M., Slooter, A. J. C., Pandharipande, P. P., Watson, P.L., Weinhouse, G.L., Nunnally, M.E., Rochwerg, B., Balas, M.C., van den Boogaard, M., Bosma, K.J., Brummel, N.E., Chanques, G., Denehy, L., Drouot, X., Fraser, G.L., Harris, J.E., … Alhazzani, W. (2018). Executive summary: Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Critical Care Medicine, 46(9). 1532-1548. doi:10.1097/CCM.0000000000003259
Filipovic-Grcic, I. F., Tonkovic, D. T., Grubisin, J. G., Peric, M. P., & Majeric Kogler, V. M. (2010). Hospital anxiety depression scale in our surgical ICU. Critical Care, 14, 499. doi:10.1186/cc8731
Finstad, K. (2010). Response interpolation and scale sensitivity: Evidence against 5 point scales. Journal of Usability Studies, 5(3), 204-110.
Gerber, S. M., Jeitziner, M.-M., Knobel, S. E. J., Mosimann, U. P., Müri, R. M., Jakob, S. M., & Nef, T. (2019). Perception and performance on a virtual reality cognitive stimulation for use in the intensive care unit: A non-randomized trial in critically ill patients. Frontiers in Medicine, 6(287), 1-10. doi:10.3389/fmed.2019.00287
Institute for Healthcare Improvement (2021). Plan-Do-Study-Act (PDSA) Worksheet. Retrieved from: http://www.ihi.org/resources/Pages/Tools/PlanDoStudyActWorksheet.aspx
Jin, W., Choo, A., Gromala, D., Shaw, C., & Squire, P. (2016). A virtual reality game for chronic pain management: A randomized, controlled clinical study. Studies in Health Technology and Informatics, 220, 154-160. doi:10.3233/978-1-61499- 625-5-154
Jones, T., Moore, T., & Choo, J. (2016). The impact of virtual reality on chronic pain. PLoS ONE, 11(12), e0167523. doi:10.1371%2Fjournal.pone.0167523
Mallari, B., Spaeth, E.K., Goh, H., & Boyd, B.S. (2019). Virtual reality as an analgesic for acute and chronic pain in adult: A systematic review and meta-analysis. Journal of Pain Research, 12, 2053-2084. doi:10.2147/jpr.s200498
McSherry, T., Atterbury, M., Gartner, S., Helmold, E., Mazzacano Searles, D., & Schulman, C. (2018). Randomized, crossover study of immersive virtual reality to decrease opioid use during painful wound care procedures in adults. Journal of Burn Care and Research, 39(2), 278-285. doi:10.1097/BCR.0000000000000589
Meghani, N., Tracy, M. F., Hadidi, N. N., & Lindquist, R. (2017). Part I: The effects of music for the symptom management of anxiety, pain, and insomnia in critically ill patients: An integrative review of current literature. Dimensions of Critical Care Nursing, 36(4), 234- 243. doi:10.1097/DCC.0000000000000254
Merriam-Webster. (2018). Definition of Virtual Reality. Retrieved from: https://www.merriam-webster.com/dictionary/virtual%20reality
Mosso-Vázquez, J. L., Gao, K., Wiederhold, B. K., & Wiederhold, M. D. (2014). Virtual reality for pain management in cardiac surgery. Cyberpsychology, Behavior, and Social Networking, 17(6), 371-378. doi:10.1089/cyber.2014.0198
Nichols, S., & Patel, H. (2002). Health and safety implications of virtual reality: A review of empirical evidence. Applied Ergonomics, 33(3), 251-271. doi:10.1016/s0003- 6870(02)00020-0
Pandya, P. G., Kim, T.E., Howard, S. K., Stary, E., Leng, J. C., Hunter, O. O., & Mariano, E. R. (2017). Virtual reality distraction decreases routine intravenous sedation and procedure related pain during postoperative adductor canal catheter insertion: A retrospective study. Korean Journal of Anesthesiology, 70(4), 439-445. doi:10.4097/kjae.2017.70.4.439
Puntillo, K. A., Max, A., Timsit, J.-F., Vignoud, L., Chanques, G., Robleda, G., Roche- Campo, F., Mancebo, J., Divatia, J.V., Soares, M., Ionescu, D.C., Grintescu, I.M., Vasiliu, I.L., Maggiore, S.M., Rusinova, K., Owczuk, R., Egerod, I., Papathanassoglou, E.D.E, Kyranou, M., … Azoulay, E. (2014). Determinants of procedural pain intensity in the intensive care unit. American Journal of Respiratory and Critical Care Medicine, 189(1), 39-47. doi:10.1164/rccm.201306- 1174OC
R Core Team (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Retrieved from: https://www.R-project.org/
Rotondi, A. J., Chelluri, L., Sirio, C., Mendelsohn, A., Schulz, R., Belle, S., Im, K., Donahoe, M., & Pinsky, M. R. (2002). Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Critical Care Medicine, 30(4), 746-752.doi:10.1097/00003246-200204000- 00004
Shahriari, M., Golshan, A., Alimohammadi, N., Abbasi, S., & Fazel, K. (2015). Effects of pain management program on the length of stay of patients with decreased level of consciousness: A clinical trial. Iranian Journal of Nursing and Midwifery Research, 20(4), 502-507. doi:10.4103/1735-9066.160996
Tashjian, V. C., Mosadeghi, S., Howard, A. R., Lopez, M., Dupuy, T., Reid, M., Martinez, B., Ahmed, S., Dailey, F., Robbins, K., Rosen, B., Fuller, G., Danovitch, I., IsHak, W., & Speigel, B. (2017). Virtual reality for management of pain in hospitalized patients: Results of a controlled trial. JMIR Mental Health, 4(1), 1-11. doi:10.2196/mental.7387
Tate, J. A., Devito Dabbs, A., Hoffman, L.A., Milbrandt, E., & Happ, M. B. (2012). Anxiety and agitation in mechanically ventilated patients. Qualitative Health Research, 22(2), 157-173. doi:10.1177/1049732311421616
Tracy, M. F., & Chlan, L. (2011). Nonpharmacological interventions to manage common symptoms in patients receiving mechanical ventilation. Critical Care Nurse, 31(3), 19-28. doi:10.4037/ccn2011653